Breakthrough discovery: How scientists are overcoming drug-resistant tuberculosis
By
Aubrey Razon
- Replies 0
Tuberculosis (TB) has long been a global health threat, especially with the rise of drug-resistant strains. But there’s a promising new development that could change the course of the fight against this deadly disease.
Could this breakthrough be the key to finally overcoming TB?
Recent advancements in medical research have brought to light three groundbreaking drug regimens that are poised to revolutionize the treatment of TB resistant to rifampin, the cornerstone antibiotic in the fight against TB.
These findings, heralded in the prestigious New England Journal of Medicine, represent a potential paradigm shift in our approach to combating drug-resistant TB.
TB remains a critical global health issue, with over a million fatalities in 2023 alone.
The World Health Organization (WHO) reports approximately 410,000 new cases of drug-resistant TB annually, many of which remain undiagnosed or untreated.
This stark reality underscores the urgent need for more effective treatment options.
The endTB clinical trial, an international endeavor, has tested five all-oral, nine-month regimens combining two newer drugs—bedaquiline and delamanid—with older medications.
Out of these, three regimens have shown success rates between 85–90 percent, surpassing the 81 percent success rate of the control group.
These results are not only promising in terms of efficacy but also in terms of reduced side effects, shorter treatment durations, and increased affordability.
The shift from older treatments, which often required painful daily injections and lengthy treatment periods, to these new pill-based combinations is a significant leap forward.
These regimens can be customized to individual patient needs, enhancing accessibility and adherence to treatment.
The endTB trial's inclusivity is noteworthy, enrolling 754 patients from diverse backgrounds and health conditions across seven countries.
This inclusivity ensures that the findings are applicable to a broad spectrum of the population, including those often left out of clinical trials.
Following the publication of a special report in August 2024, the WHO has incorporated these three new regimens into its list of recommended treatments for drug-resistant TB.
The next phase will focus on ensuring that these regimens are widely available and accessible to those in need.
Carole Mitnick, the trial's co-principal investigator, emphasized the significance of this partnership among NGOs, ministries of health, and academic partners in making lifesaving care more accessible.
The trial also addressed critical questions regarding the optimal use of new drugs to shorten and simplify treatment while maintaining effectiveness.
 Have you or someone you know been affected by TB? Share your stories in the comments below. Let's foster a community where we can learn from each other and support those facing health challenges.
Have you or someone you know been affected by TB? Share your stories in the comments below. Let's foster a community where we can learn from each other and support those facing health challenges.
Could this breakthrough be the key to finally overcoming TB?
Recent advancements in medical research have brought to light three groundbreaking drug regimens that are poised to revolutionize the treatment of TB resistant to rifampin, the cornerstone antibiotic in the fight against TB.
These findings, heralded in the prestigious New England Journal of Medicine, represent a potential paradigm shift in our approach to combating drug-resistant TB.
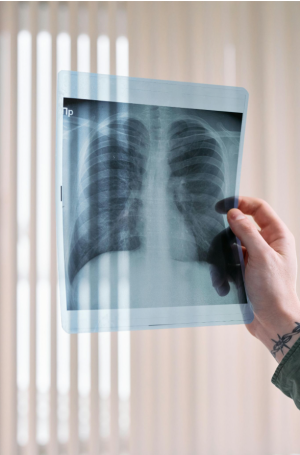
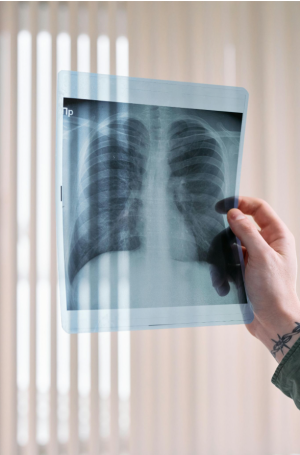
The endTB trial has provided evidence that can change the treatment landscape for TB. Image source: cottonbro studio/Pexels.
TB remains a critical global health issue, with over a million fatalities in 2023 alone.
The World Health Organization (WHO) reports approximately 410,000 new cases of drug-resistant TB annually, many of which remain undiagnosed or untreated.
This stark reality underscores the urgent need for more effective treatment options.
The endTB clinical trial, an international endeavor, has tested five all-oral, nine-month regimens combining two newer drugs—bedaquiline and delamanid—with older medications.
Out of these, three regimens have shown success rates between 85–90 percent, surpassing the 81 percent success rate of the control group.
These results are not only promising in terms of efficacy but also in terms of reduced side effects, shorter treatment durations, and increased affordability.
The shift from older treatments, which often required painful daily injections and lengthy treatment periods, to these new pill-based combinations is a significant leap forward.
These regimens can be customized to individual patient needs, enhancing accessibility and adherence to treatment.
The endTB trial's inclusivity is noteworthy, enrolling 754 patients from diverse backgrounds and health conditions across seven countries.
This inclusivity ensures that the findings are applicable to a broad spectrum of the population, including those often left out of clinical trials.
Following the publication of a special report in August 2024, the WHO has incorporated these three new regimens into its list of recommended treatments for drug-resistant TB.
The next phase will focus on ensuring that these regimens are widely available and accessible to those in need.
Carole Mitnick, the trial's co-principal investigator, emphasized the significance of this partnership among NGOs, ministries of health, and academic partners in making lifesaving care more accessible.
The trial also addressed critical questions regarding the optimal use of new drugs to shorten and simplify treatment while maintaining effectiveness.
Key Takeaways
- International clinical trials have found three new highly effective drug regimens for treating drug-resistant tuberculosis (TB), which is a significant breakthrough for global health.
- The treatments have success rates between 85–90 percent, are less toxic, have shorter treatment durations, and are more affordable than previous options.
- The new all-oral regimens combine two newer drugs, bedaquiline and delamanid, with older medications, and have been included in the WHO's recommended treatment options for drug-resistant TB.
- The endTB trial has provided evidence that can change the treatment landscape for TB, impacting patients worldwide, including those in diverse populations like children and individuals with HIV or hepatitis C.