Can rheumatoid arthritis be stopped before it starts?
By
Veronica E.
- Replies 0
Imagine a future where rheumatoid arthritis (RA)—a disease that stiffens joints, drains energy, and reshapes lives—never gets the chance to begin.
For the millions of Americans living with the possibility of RA, that future may not be as far off as it once seemed.
Researchers have uncovered new evidence that the disease could be prevented long before painful symptoms ever appear.
This discovery could change not only how RA is treated, but also how it is stopped.
For older adults and families who know the toll RA can take, the findings carry both hope and urgency.

The silent beginnings of RA
For years, RA was often thought of as a condition that revealed itself suddenly when joint swelling and pain began.
But new research shows the disease starts much earlier.
Scientists from the Allen Institute of Immunology, the University of California San Diego, the University of Colorado Anschutz Medical Campus, and the Benaroya Research Institute spent seven years studying people at risk.
Published in Science Translational Medicine, their findings reveal the immune system undergoes major changes years before RA’s first noticeable signs.
Also read: Swollen fingers? Here’s what they might be telling you
The pre-RA stage: a critical window
Researchers followed people who carried ACPA antibodies—markers known to signal higher risk for RA.
Though these individuals felt healthy, their immune systems were already showing abnormal behavior.
The study identified widespread inflammation, dysfunction in immune cells, and even “reprogramming” of naïve T cells that should normally remain neutral.
These cells were instead primed in ways that could ignite RA.
It is as though the body was preparing for a battle long before it began.
Dr. Kevin Deane, a rheumatology professor at CU Anschutz, explained the potential: “If we find ways to prevent the first swollen joints in RA, or even reset the immune system in an at-risk stage, this could lead to people never getting full-blown RA—or having a much milder form of disease.”
Also read: Think sunscreen is enough? These 4 medications could still leave you vulnerable
The weight of RA
Rheumatoid arthritis affects about 1.5 million Americans, often appearing in midlife and beyond.
It is more than painful joints—it can cause lasting deformities, severe fatigue, and even damage to organs.
Managing RA also requires costly treatments and lifelong care, with billions spent each year on medications and lost productivity.
Because current therapies focus on controlling disease after diagnosis, the possibility of prevention offers a profound shift in care.
Also read: Can you reverse osteoporosis? The surprising truth about stronger bones after 60
Toward prevention instead of reaction
The research points to a new approach where doctors could identify who is at risk and act before joints are ever damaged.
This might include:
Dr. Deane compared it to cardiovascular care: “Someone gets a blood test (like a cholesterol level, or anti-CCP) that helps predict risk and then is given an intervention (like a cholesterol-lowering medication, or an RA-directed therapy) to help reduce the risk of a heart attack (or full-blown RA).”
Also read: Are these hidden health risks affecting you? What one doctor says you should know
What lies ahead
No drug yet exists to stop RA, but early trials show that delaying onset may be possible.
With the immune system changes now mapped out, future trials may be more effective.
As Allen Institute investigator Mark Gillespie noted, “Our team discovered that during this at-risk period where individuals look and feel healthy, their immune systems are dramatically different.
This could help us identify who will get RA and, more importantly, how to stop it.”
Also read: Could a simple stride change help ease arthritis pain?
Steps you can take now
For those with a family history of RA or who test positive for anti-CCP antibodies, there are ways to stay proactive:
This research reflects a broader shift in medicine toward prevention, not just treatment.
For anyone concerned about RA, it brings hope that the disease might one day be stopped before it begins.
Read next:

Have you or someone close to you experienced RA? Do you think prevention strategies should become part of routine care? Share your thoughts—we’d love to hear how this breakthrough resonates with you.
For the millions of Americans living with the possibility of RA, that future may not be as far off as it once seemed.
Researchers have uncovered new evidence that the disease could be prevented long before painful symptoms ever appear.
This discovery could change not only how RA is treated, but also how it is stopped.
For older adults and families who know the toll RA can take, the findings carry both hope and urgency.

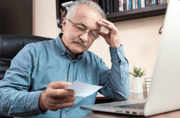
New research offers hope that rheumatoid arthritis may one day be prevented before painful symptoms ever begin. Image Source: Pexels / Towfiqu barbhuiya.
The silent beginnings of RA
For years, RA was often thought of as a condition that revealed itself suddenly when joint swelling and pain began.
But new research shows the disease starts much earlier.
Scientists from the Allen Institute of Immunology, the University of California San Diego, the University of Colorado Anschutz Medical Campus, and the Benaroya Research Institute spent seven years studying people at risk.
Published in Science Translational Medicine, their findings reveal the immune system undergoes major changes years before RA’s first noticeable signs.
Also read: Swollen fingers? Here’s what they might be telling you
The pre-RA stage: a critical window
Researchers followed people who carried ACPA antibodies—markers known to signal higher risk for RA.
Though these individuals felt healthy, their immune systems were already showing abnormal behavior.
The study identified widespread inflammation, dysfunction in immune cells, and even “reprogramming” of naïve T cells that should normally remain neutral.
These cells were instead primed in ways that could ignite RA.
It is as though the body was preparing for a battle long before it began.
Dr. Kevin Deane, a rheumatology professor at CU Anschutz, explained the potential: “If we find ways to prevent the first swollen joints in RA, or even reset the immune system in an at-risk stage, this could lead to people never getting full-blown RA—or having a much milder form of disease.”
Also read: Think sunscreen is enough? These 4 medications could still leave you vulnerable
The weight of RA
Rheumatoid arthritis affects about 1.5 million Americans, often appearing in midlife and beyond.
It is more than painful joints—it can cause lasting deformities, severe fatigue, and even damage to organs.
Managing RA also requires costly treatments and lifelong care, with billions spent each year on medications and lost productivity.
Because current therapies focus on controlling disease after diagnosis, the possibility of prevention offers a profound shift in care.
Also read: Can you reverse osteoporosis? The surprising truth about stronger bones after 60
Toward prevention instead of reaction
The research points to a new approach where doctors could identify who is at risk and act before joints are ever damaged.
This might include:
- Early detection: Blood tests for anti-CCP antibodies already help reveal risk. With these new immune system findings, testing could become more precise.
- Personalized monitoring: Not everyone with risk markers develops RA. The new clues may help distinguish who is most likely to progress.
- Targeted prevention: Understanding immune shifts before RA develops could lead to treatments that “reset” the immune system before lasting damage occurs.
Dr. Deane compared it to cardiovascular care: “Someone gets a blood test (like a cholesterol level, or anti-CCP) that helps predict risk and then is given an intervention (like a cholesterol-lowering medication, or an RA-directed therapy) to help reduce the risk of a heart attack (or full-blown RA).”
Also read: Are these hidden health risks affecting you? What one doctor says you should know
What lies ahead
No drug yet exists to stop RA, but early trials show that delaying onset may be possible.
With the immune system changes now mapped out, future trials may be more effective.
As Allen Institute investigator Mark Gillespie noted, “Our team discovered that during this at-risk period where individuals look and feel healthy, their immune systems are dramatically different.
This could help us identify who will get RA and, more importantly, how to stop it.”
Also read: Could a simple stride change help ease arthritis pain?
Steps you can take now
For those with a family history of RA or who test positive for anti-CCP antibodies, there are ways to stay proactive:
- Know your family history. Tell your doctor if relatives have RA.
- Ask about blood tests. If concerned, discuss RA markers like anti-CCP with your healthcare provider.
- Stay informed. Research is moving quickly—stay updated and check in with your doctor about new prevention strategies.
This research reflects a broader shift in medicine toward prevention, not just treatment.
For anyone concerned about RA, it brings hope that the disease might one day be stopped before it begins.
Read next:
- Suffering from joint pain? Discover 5 foods that could provide incredible relief!
- Consider these 4 doctor-approved tips to help maintain strong, healthy bones
- Reverse your back pain and supercharge your brainpower with this counterintuitive trick!
Key Takeaways
- Researchers discovered that rheumatoid arthritis can begin developing years before symptoms appear, with clear immune system changes in at-risk individuals.
- The study tracked people with ACPA antibodies and found widespread inflammation and altered immune cells, even in those who felt healthy.
- Doctors may one day use these findings to detect who is most likely to develop RA and intervene before damage begins.
- Although no preventive drug exists yet, early trials and new research bring hope for proactive strategies to reduce RA risk.
Have you or someone close to you experienced RA? Do you think prevention strategies should become part of routine care? Share your thoughts—we’d love to hear how this breakthrough resonates with you.