CVS expands program to help Medicare members avoid costly hospital readmissions
- Replies 0
If you’re on Medicare—or caring for someone who is—you probably know how tough the weeks after a hospital stay can be.
Discharge papers are often confusing, medications can be overwhelming, and arranging follow-up appointments isn’t always simple.
For many, this stressful period can turn into another trip back to the hospital.
But a new effort from one of the nation’s biggest healthcare companies could help change that experience.
Imagine this: You’re being discharged from the hospital, and instead of being handed a stack of paperwork and a “good luck,” you’re introduced to a nurse who’s there to guide you through the next steps.
That’s the heart of Aetna’s new approach. For Medicare Advantage members—those 65 and older, or living with disabilities—Aetna-employed nurses will be assigned to help navigate the tricky transition from hospital to home or nursing facility.
These nurses aren’t just checking in with a phone call. They’re coordinating in-home care, making sure you have a ride to your follow-up appointments, and helping you understand your medications and care plan.
As Dr. Ben Kornitzer, Aetna’s chief medical officer, puts it: “Our goal is to literally have a nurse at the bedside with that member, with that family, beginning to think through what their care journey should look like.”
This expansion comes on the heels of a major policy change from the Centers for Medicare & Medicaid Services (CMS).
Starting in 2027, hospitals will be penalized for higher-than-expected readmissions among Medicare Advantage members—not just those on traditional Medicare.
That means hospitals and insurers alike have a bigger incentive than ever to keep patients healthy and out of the hospital.
But it’s not just about dollars and cents. Hospital readmissions are tough on patients—physically, emotionally, and financially.
Each return trip can mean more stress, more risk of complications, and more time away from the comforts of home and family.
In 2023, a whopping 75% of hospitals subject to the CMS readmission rule faced penalties, according to research by the Advisory Board. That’s a lot of hospitals—and a lot of patients caught in the cycle of readmission.
The American Hospital Association has pushed back, arguing that hospitals shouldn’t be penalized for issues like insurance coverage delays or denials.
But the message from CMS is clear: Everyone involved in your care needs to work together to keep you healthy after you leave the hospital.
Also read: Rite Aid turns to CVS to save dozens of stores from closing for good
By the end of this year, Aetna’s expanded program will be up and running in 10 hospitals across the country.
Some of the first to join include AdventHealth Shawnee Mission in Kansas City, Houston Methodist in Texas, and WakeMed Health & Hospitals in Raleigh, North Carolina.
If you’re an Aetna Medicare Advantage member in these areas, you could soon see a nurse at your bedside, ready to help you chart a smoother path home.
Also read: Don't miss out: Four settlements with deadlines you need to know
For many older Americans, the days and weeks after a hospital stay are some of the most vulnerable.
Having a dedicated nurse to coordinate care, answer questions, and make sure nothing falls through the cracks could be a game-changer.
As Sadhna Paralkar, a senior vice president at health consultancy Segal, notes: “Sometimes the health plan is more helpful in giving discharge instructions, because they have a vested interest in keeping the patient better.”
And it’s not just about avoiding another hospital stay. It’s about peace of mind—knowing you have someone in your corner, helping you get back on your feet.
CVS Health says this is just the beginning. The company plans to push for similar programs in more hospitals and communities, aiming to make this kind of hands-on support the new normal for Medicare Advantage members.
This shift reflects a broader trend in healthcare: moving away from a “one-and-done” approach to hospital care, and toward a more holistic, ongoing partnership between patients, providers, and insurers.
It’s a recognition that good health doesn’t end at the hospital door—and that a little extra support can make all the difference.
Read next:

Have you or a loved one experienced a tough transition from hospital to home? Would having a nurse at your bedside have made a difference? Do you have tips for managing post-hospital care, or questions about Medicare Advantage plans?
Discharge papers are often confusing, medications can be overwhelming, and arranging follow-up appointments isn’t always simple.
For many, this stressful period can turn into another trip back to the hospital.
But a new effort from one of the nation’s biggest healthcare companies could help change that experience.
Imagine this: You’re being discharged from the hospital, and instead of being handed a stack of paperwork and a “good luck,” you’re introduced to a nurse who’s there to guide you through the next steps.
That’s the heart of Aetna’s new approach. For Medicare Advantage members—those 65 and older, or living with disabilities—Aetna-employed nurses will be assigned to help navigate the tricky transition from hospital to home or nursing facility.
These nurses aren’t just checking in with a phone call. They’re coordinating in-home care, making sure you have a ride to your follow-up appointments, and helping you understand your medications and care plan.
As Dr. Ben Kornitzer, Aetna’s chief medical officer, puts it: “Our goal is to literally have a nurse at the bedside with that member, with that family, beginning to think through what their care journey should look like.”
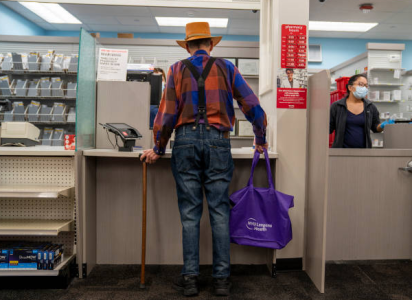
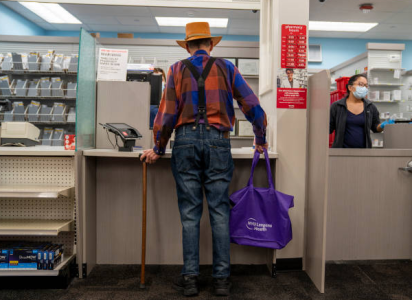
The goal is to reduce readmissions, which are not only costly but also emotionally and physically draining. Image source: Getty Images
This expansion comes on the heels of a major policy change from the Centers for Medicare & Medicaid Services (CMS).
Starting in 2027, hospitals will be penalized for higher-than-expected readmissions among Medicare Advantage members—not just those on traditional Medicare.
That means hospitals and insurers alike have a bigger incentive than ever to keep patients healthy and out of the hospital.
But it’s not just about dollars and cents. Hospital readmissions are tough on patients—physically, emotionally, and financially.
Each return trip can mean more stress, more risk of complications, and more time away from the comforts of home and family.
In 2023, a whopping 75% of hospitals subject to the CMS readmission rule faced penalties, according to research by the Advisory Board. That’s a lot of hospitals—and a lot of patients caught in the cycle of readmission.
The American Hospital Association has pushed back, arguing that hospitals shouldn’t be penalized for issues like insurance coverage delays or denials.
But the message from CMS is clear: Everyone involved in your care needs to work together to keep you healthy after you leave the hospital.
Also read: Rite Aid turns to CVS to save dozens of stores from closing for good
By the end of this year, Aetna’s expanded program will be up and running in 10 hospitals across the country.
Some of the first to join include AdventHealth Shawnee Mission in Kansas City, Houston Methodist in Texas, and WakeMed Health & Hospitals in Raleigh, North Carolina.
If you’re an Aetna Medicare Advantage member in these areas, you could soon see a nurse at your bedside, ready to help you chart a smoother path home.
Also read: Don't miss out: Four settlements with deadlines you need to know
For many older Americans, the days and weeks after a hospital stay are some of the most vulnerable.
Having a dedicated nurse to coordinate care, answer questions, and make sure nothing falls through the cracks could be a game-changer.
As Sadhna Paralkar, a senior vice president at health consultancy Segal, notes: “Sometimes the health plan is more helpful in giving discharge instructions, because they have a vested interest in keeping the patient better.”
And it’s not just about avoiding another hospital stay. It’s about peace of mind—knowing you have someone in your corner, helping you get back on your feet.
CVS Health says this is just the beginning. The company plans to push for similar programs in more hospitals and communities, aiming to make this kind of hands-on support the new normal for Medicare Advantage members.
This shift reflects a broader trend in healthcare: moving away from a “one-and-done” approach to hospital care, and toward a more holistic, ongoing partnership between patients, providers, and insurers.
It’s a recognition that good health doesn’t end at the hospital door—and that a little extra support can make all the difference.
Read next:
- Medicare bill could protect home health care access for millions
- Missing these Medicare deadlines could drain your wallet—here’s how to stay on track
Key Takeaways
- CVS Health’s Aetna is expanding a program that pairs Medicare Advantage members with nurses to help reduce costly hospital readmissions and improve patient health outcomes.
- The program supports patients aged 65 and over as they move from hospital to home or into care facilities, with nurses coordinating in-home care and arranging follow-up appointments and transport.
- The expansion comes after a government rule including Medicare Advantage patients in hospital readmission penalty calculations from 2027, which has been criticized by the American Hospital Association.
- CVS plans to introduce the program in 10 hospitals before the year’s end, aiming to benefit both Aetna and healthcare providers, with hopes to launch similar initiatives in the future.