Older adults face hidden risks from concussions more often than you think
- Replies 0
When you hear the word “concussion,” you might picture a football player staggering off the field or a daredevil cyclist taking a tumble.
But there’s a surprising truth: the most common cause of concussions isn’t a sports injury or a car accident. And for Americans over 60, that means concussions are a lot closer to home than you might think.
Let’s pull back the curtain on concussions, especially as they relate to older adults. Whether you’re an active grandparent, a gardening enthusiast, or just someone who wants to stay sharp and safe, understanding the risks, symptoms, and recovery process is essential.
According to the Centers for Disease Control and Prevention (CDC), adults 65 and older experience a staggering 36 million falls each year in the United States. That’s not a typo—36 million!
As we age, changes in balance, vision, muscle strength, and even medications can make us more prone to losing our footing. And when a fall happens, the risk of hitting your head and sustaining a concussion goes up.
But here’s the kicker: many older adults don’t realize they’ve had a concussion. Maybe you brushed off a tumble in the garden or a slip in the kitchen because you felt “mostly fine.” Or perhaps you chalked up some forgetfulness or dizziness to “just getting older.”
A concussion is a mild traumatic brain injury (TBI) that happens when your brain gets jolted inside your skull—think of it like your brain getting a quick shake.
This can happen from a direct blow to the head, face, or neck, or even from a jolt to the body that whips your head back and forth.
Dr. Jonathan Rasouli, a neurosurgeon at Northwell Health, explains that a concussion triggers a sudden rush of brain chemicals called neurotransmitters.
This chemical surge can temporarily scramble your thinking, speech, judgment, and awareness. You might feel “off,” confused, or just not quite yourself.
Concussion symptoms can show up right away, or they might sneak in hours, days, or even weeks after a fall.
It’s tempting to brush off a fall—especially if you’re able to get up and feel okay. But here’s our advice: err on the side of caution.
If you hit your head, go to the emergency room (ER) for a checkup, even if you think it’s “no big deal.” Some injuries, like brain bleeds, can be life-threatening if missed.
In the ER, doctors will check your cognitive function (asking your name, the date, and where you are) and may order imaging tests like X-rays, CT scans, or MRIs.
While these scans can’t diagnose a concussion directly, they can rule out more serious problems like bleeding or swelling in the brain.
And don’t forget to tell your primary care doctor about your fall and any ER visits. This helps them connect the dots if you develop new symptoms later on and prevents them from misattributing concussion symptoms to “just aging.”
The good news: most people recover fully from a single concussion within a couple of weeks. The brain is remarkably resilient, even as we age.
But recovery can take longer for older adults, and having had previous concussions or mental health issues (like depression or anxiety) can slow things down.
Some people develop what’s called “post-concussion syndrome,” where symptoms like headaches, fatigue, memory problems, and sleep issues linger for months.
In most cases, these symptoms improve within a month or two, but sometimes they can last up to a year.
Also read: What you do right after a fall can prevent serious complications—ER doctors explain
Also read: This enjoyable hobbies may be the key to better brain health, according to scientists
If your symptoms don’t improve after a few weeks, or if you’re struggling with memory, balance, vision, or mood, ask your doctor for a referral to a head injury specialist. Rehabilitation options might include:
Read next: Could this at-home test help detect memory decline before it starts?

Have you or a loved one experienced a concussion? Did you notice symptoms right away, or did they sneak up on you? What helped you recover?
But there’s a surprising truth: the most common cause of concussions isn’t a sports injury or a car accident. And for Americans over 60, that means concussions are a lot closer to home than you might think.
Let’s pull back the curtain on concussions, especially as they relate to older adults. Whether you’re an active grandparent, a gardening enthusiast, or just someone who wants to stay sharp and safe, understanding the risks, symptoms, and recovery process is essential.
According to the Centers for Disease Control and Prevention (CDC), adults 65 and older experience a staggering 36 million falls each year in the United States. That’s not a typo—36 million!
As we age, changes in balance, vision, muscle strength, and even medications can make us more prone to losing our footing. And when a fall happens, the risk of hitting your head and sustaining a concussion goes up.
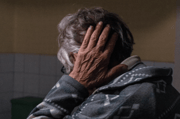
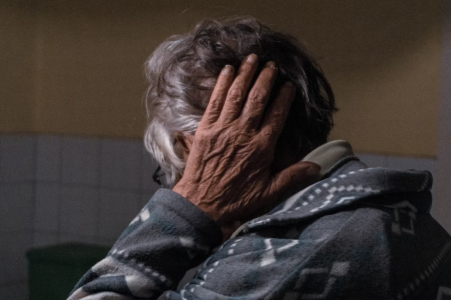
But here’s the kicker: many older adults don’t realize they’ve had a concussion. Maybe you brushed off a tumble in the garden or a slip in the kitchen because you felt “mostly fine.” Or perhaps you chalked up some forgetfulness or dizziness to “just getting older.”
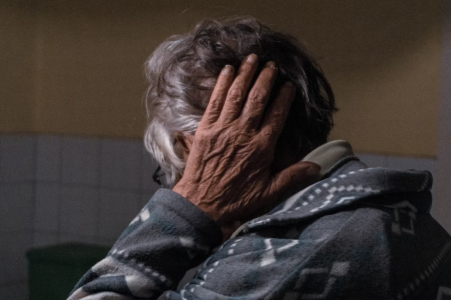
Concussions can be sneaky, and their symptoms often overlap with normal aging. Image source: Jan Krivec / Unsplash
A concussion is a mild traumatic brain injury (TBI) that happens when your brain gets jolted inside your skull—think of it like your brain getting a quick shake.
This can happen from a direct blow to the head, face, or neck, or even from a jolt to the body that whips your head back and forth.
Dr. Jonathan Rasouli, a neurosurgeon at Northwell Health, explains that a concussion triggers a sudden rush of brain chemicals called neurotransmitters.
This chemical surge can temporarily scramble your thinking, speech, judgment, and awareness. You might feel “off,” confused, or just not quite yourself.
Concussion symptoms can show up right away, or they might sneak in hours, days, or even weeks after a fall.
Here’s what to watch for:
- Cognitive changes: Trouble with memory (short- or long-term), concentration, or feeling mentally sluggish.
- Emotional changes: Feeling anxious, irritable, sad, or unusually angry.
- Physical symptoms: Headaches, dizziness, balance problems, nausea or vomiting, sensitivity to light or noise, or a feeling of “pressure” in the head.
- Sleep disturbances: Insomnia, sleeping more than usual, or trouble staying asleep.
It’s tempting to brush off a fall—especially if you’re able to get up and feel okay. But here’s our advice: err on the side of caution.
If you hit your head, go to the emergency room (ER) for a checkup, even if you think it’s “no big deal.” Some injuries, like brain bleeds, can be life-threatening if missed.
In the ER, doctors will check your cognitive function (asking your name, the date, and where you are) and may order imaging tests like X-rays, CT scans, or MRIs.
While these scans can’t diagnose a concussion directly, they can rule out more serious problems like bleeding or swelling in the brain.
And don’t forget to tell your primary care doctor about your fall and any ER visits. This helps them connect the dots if you develop new symptoms later on and prevents them from misattributing concussion symptoms to “just aging.”
The good news: most people recover fully from a single concussion within a couple of weeks. The brain is remarkably resilient, even as we age.
But recovery can take longer for older adults, and having had previous concussions or mental health issues (like depression or anxiety) can slow things down.
Some people develop what’s called “post-concussion syndrome,” where symptoms like headaches, fatigue, memory problems, and sleep issues linger for months.
In most cases, these symptoms improve within a month or two, but sometimes they can last up to a year.
Also read: What you do right after a fall can prevent serious complications—ER doctors explain
The road to recovery
- Rest is best (at first): Take it easy for the first 1-2 days after a concussion. Limit screen time, avoid loud noises and bright lights, and get plenty of sleep.
- Gradual return to activity: After a couple of days, start easing back into your normal routine as you feel able. Studies show that gentle activity can actually speed up recovery.
- Pain management: Over-the-counter pain relievers can help with headaches, but check with your doctor first.
- Monitor your symptoms: Keep a journal of how you’re feeling. If symptoms persist or worsen, let your doctor know.
Also read: This enjoyable hobbies may be the key to better brain health, according to scientists
If your symptoms don’t improve after a few weeks, or if you’re struggling with memory, balance, vision, or mood, ask your doctor for a referral to a head injury specialist. Rehabilitation options might include:
- Cognitive therapy: To boost memory, attention, and processing speed.
- Vestibular therapy: For balance and dizziness issues.
- Vision therapy: For double vision or other visual problems.
- Brain training programs: Evidence-based exercises to help your brain rewire and recover.
Read next: Could this at-home test help detect memory decline before it starts?
Key Takeaways
- Older adults are particularly at risk of concussion because falls are the most common cause, and people aged 65 and over are more likely to have a fall.
- Symptoms of concussion can be subtle or mistaken for normal age-related issues, including confusion, memory problems, balance difficulties, headaches, and changes in mood or sleep.
- It’s important for older people who hit their head in a fall to seek medical attention, even if they feel fine at first, as some symptoms can take days or weeks to appear.
- Recovery from a concussion in older adults may take longer, but most people fully recover; if symptoms persist, specialist therapies like cognitive, vestibular, or vision rehabilitation may help.