Ten patients, no more insulin—are we getting closer to curing diabetes?
By
Veronica E.
- Replies 0
Disclaimer: The information provided in this article is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult your physician or other qualified healthcare providers with any questions you may have regarding a medical condition or before making any changes to your health regimen.
A recent medical breakthrough is giving hope to millions of people living with diabetes.
It started quietly—with just a small group of patients and a treatment that many thought wouldn’t be possible in their lifetime.
But after just one year, the results are turning heads across the medical world.
The therapy involves a lab-grown solution, years in the making, and the outcomes so far suggest a dramatic shift in how diabetes may be treated in the future.
Let’s take a closer look at what happened, who it could help, and what’s still ahead.

For people with type 1 diabetes, daily life often means a constant balancing act of insulin injections, glucose monitoring, and the ever-present risk of a dangerous blood sugar drop.
It’s not just inconvenient—it can be life-threatening.
About 30% of those with type 1 develop hypoglycemic unawareness, a condition where the body no longer signals when blood sugar drops too low, putting people at risk of sudden fainting, hospital visits, or worse.
That’s why the early results from a new therapy, Zimislecel, are so encouraging.
Developed by Vertex Pharmaceuticals, this experimental treatment uses stem cells that are engineered in a lab to become insulin-producing islet cells—the very ones the pancreas fails to make in type 1 diabetes.
Unlike traditional transplants that rely on organ donors, these lab-grown cells offer the potential for a renewable and more widely available solution.
Doctors inject the lab-created cells directly into the patient’s liver, where they take hold and begin producing insulin naturally.
In a recent trial involving 12 patients with severe type 1 diabetes and hypoglycemic unawareness, the results were remarkable:
One participant, 36-year-old Amanda Smith from London, said it felt like getting her life back.
Six months after her treatment, she was off insulin completely.
Until now, islet cell transplants depended on donor tissue—a method limited by supply and rejection risks.
Zimislecel sidesteps both by using stem cells grown in controlled lab conditions, allowing for broader application.
The main hurdle now? Since these new cells are technically foreign to the body, patients need immune-suppressing medications to prevent rejection.
That said, researchers are working to reduce or eliminate this requirement over time. If they succeed, the treatment could become safer, more accessible, and more appealing for long-term use.
Stories from the trial highlight just how life-changing this therapy can be.
Marlaina Goedel, a 30-year-old mom from Illinois, had been dealing with type 1 diabetes since she was five. Within a month of receiving her infusion, her blood sugar stabilized, and she no longer needed insulin. “I am cured,” she said, a sentence she never thought she’d say.
Brian Sheton, the first patient to receive the therapy in 2021, was cured of his type 1 diabetes after years of dangerous blood sugar crashes.
He later passed away due to dementia symptoms that began before his treatment.
As exciting as this is, the therapy is still in its early stages.
This first trial was small and focused on people with a very specific—and severe—form of diabetes.
Larger studies will be needed to confirm these results and understand how the treatment might work for broader populations.
Researchers are optimistic. Dr. Trevor Reichman, one of the study’s co-authors, called the trial a major milestone. He noted that for the first time, scientists have shown that a single, safe procedure can biologically replace insulin function—a long-standing goal in diabetes treatment.
The developers hope to seek FDA approval within the next five years.
While this treatment is currently aimed at type 1 diabetes, the science behind it may eventually be applied more widely.
Type 2 diabetes—which affects over 32 million Americans—is typically managed through lifestyle changes and oral medications.
But as stem cell-based approaches advance, similar strategies might one day be adapted to help people with type 2 as well.
Zimislecel is still new, but it represents a powerful symbol of progress for the diabetes community.
After decades of daily management and unmet promises, this breakthrough is offering real, measurable change—at least for a few lucky patients so far.
And while there’s more work to be done, the potential is enormous.
Read next: This meal trick has people rethinking how they eat

Have you or someone you love been living with diabetes? What do you think about this new treatment? Are you hopeful or cautious about where the science is headed?
Share your experiences and thoughts in the comments. We’d love to hear your stories—and keep the conversation going as this new chapter in diabetes care unfolds.
A recent medical breakthrough is giving hope to millions of people living with diabetes.
It started quietly—with just a small group of patients and a treatment that many thought wouldn’t be possible in their lifetime.
But after just one year, the results are turning heads across the medical world.
The therapy involves a lab-grown solution, years in the making, and the outcomes so far suggest a dramatic shift in how diabetes may be treated in the future.
Let’s take a closer look at what happened, who it could help, and what’s still ahead.

A groundbreaking new treatment is giving some people with type 1 diabetes a chance to live without daily insulin for the first time in decades. Image Source: YouTube / CNBC.
A new chapter in diabetes care
For people with type 1 diabetes, daily life often means a constant balancing act of insulin injections, glucose monitoring, and the ever-present risk of a dangerous blood sugar drop.
It’s not just inconvenient—it can be life-threatening.
About 30% of those with type 1 develop hypoglycemic unawareness, a condition where the body no longer signals when blood sugar drops too low, putting people at risk of sudden fainting, hospital visits, or worse.
That’s why the early results from a new therapy, Zimislecel, are so encouraging.
Developed by Vertex Pharmaceuticals, this experimental treatment uses stem cells that are engineered in a lab to become insulin-producing islet cells—the very ones the pancreas fails to make in type 1 diabetes.
Unlike traditional transplants that rely on organ donors, these lab-grown cells offer the potential for a renewable and more widely available solution.
Also read: The overlooked drink that can help you stay hydrated with diabetes, say dietitians
How the treatment works
Doctors inject the lab-created cells directly into the patient’s liver, where they take hold and begin producing insulin naturally.
In a recent trial involving 12 patients with severe type 1 diabetes and hypoglycemic unawareness, the results were remarkable:
- 10 of the 12 patients stopped needing insulin entirely within a year of treatment
- The other two saw a significant reduction in insulin use
- Blood sugar control improved, with patients spending over 93% of the day in a healthy glucose range
- Dangerous post-meal spikes and drops all but disappeared
One participant, 36-year-old Amanda Smith from London, said it felt like getting her life back.
Six months after her treatment, she was off insulin completely.
Also read: Could this simple diet trick lower your blood pressure—even if you have diabetes?
A scientific leap decades in the making
Until now, islet cell transplants depended on donor tissue—a method limited by supply and rejection risks.
Zimislecel sidesteps both by using stem cells grown in controlled lab conditions, allowing for broader application.
The main hurdle now? Since these new cells are technically foreign to the body, patients need immune-suppressing medications to prevent rejection.
That said, researchers are working to reduce or eliminate this requirement over time. If they succeed, the treatment could become safer, more accessible, and more appealing for long-term use.
Also read: You’re probably not getting enough of this diabetes-fighting nutrient
Real lives, real transformations
Stories from the trial highlight just how life-changing this therapy can be.
Marlaina Goedel, a 30-year-old mom from Illinois, had been dealing with type 1 diabetes since she was five. Within a month of receiving her infusion, her blood sugar stabilized, and she no longer needed insulin. “I am cured,” she said, a sentence she never thought she’d say.
Brian Sheton, the first patient to receive the therapy in 2021, was cured of his type 1 diabetes after years of dangerous blood sugar crashes.
He later passed away due to dementia symptoms that began before his treatment.
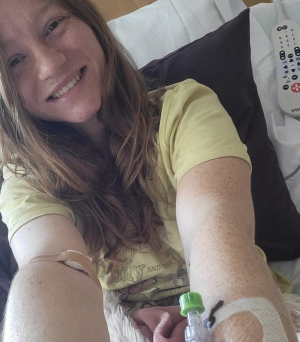
Diagnosed at just five years old, Marlaina Goedel (30) spent decades fearing each day—but after her islet cell transplant, she finally feels free. Image Source: The Daily Mail / Marlaina Goedel.
Also read: Is your breakfast drink raising your risk of diabetes? New research suggests it might
What happens next?
As exciting as this is, the therapy is still in its early stages.
This first trial was small and focused on people with a very specific—and severe—form of diabetes.
Larger studies will be needed to confirm these results and understand how the treatment might work for broader populations.
Researchers are optimistic. Dr. Trevor Reichman, one of the study’s co-authors, called the trial a major milestone. He noted that for the first time, scientists have shown that a single, safe procedure can biologically replace insulin function—a long-standing goal in diabetes treatment.
The developers hope to seek FDA approval within the next five years.
Also read: Breakthrough in prostate cancer treatment: What every patient needs to know about this game-changing discovery
Could this help those with type 2 diabetes?
While this treatment is currently aimed at type 1 diabetes, the science behind it may eventually be applied more widely.
Type 2 diabetes—which affects over 32 million Americans—is typically managed through lifestyle changes and oral medications.
But as stem cell-based approaches advance, similar strategies might one day be adapted to help people with type 2 as well.
Also read: Avoid these breakfast mistakes that can secretly spike your blood sugar levels!
A reason to feel hopeful
Zimislecel is still new, but it represents a powerful symbol of progress for the diabetes community.
After decades of daily management and unmet promises, this breakthrough is offering real, measurable change—at least for a few lucky patients so far.
And while there’s more work to be done, the potential is enormous.
Read next: This meal trick has people rethinking how they eat
Key Takeaways
- A new stem cell-based therapy called Zimislecel helped 10 out of 12 patients with type 1 diabetes stop taking insulin after one year.
- The treatment involves injecting lab-grown pancreatic islet cells into the liver, enabling the body to produce insulin naturally.
- All patients had hypoglycemic unawareness, a serious condition where blood sugar drops can happen without warning.
- While patients must currently take immune-suppressing drugs, researchers hope to make future versions of the therapy safer and more widely available.
Have you or someone you love been living with diabetes? What do you think about this new treatment? Are you hopeful or cautious about where the science is headed?
Share your experiences and thoughts in the comments. We’d love to hear your stories—and keep the conversation going as this new chapter in diabetes care unfolds.






